Understanding Lymph Node Ultrasound: The Significance Of The Short Axis / Fatty Hilum
Home | Cervical Lymph Nodes – Cervical Lymphadenopathy | Lymph Node Ultrasound: Significance of Short Axis and Fatty Hilum

Medically Reviewed By:
Dr Leslie Koh
M.B;B.S. (Singapore), MRCS (ENT) Edinburgh, M. Med (ORL), FAMS
What Is A Neck Ultrasound?
The procedure for a neck ultrasound, often used for evaluating cervical lymph nodes, is a non-invasive, painless investigation that provides valuable information about the structures in the neck. This is how a neck ultrasound is typically performed:
Preparation: The patient is usually asked to remove any jewelry or other items from around the neck area. The patient is then positioned lying down on the examination table, with a pillow placed under their shoulders to hyperextend the neck, providing better access and visibility of the neck structures.
Applying the Gel: The sonographer, a trained healthcare professional who performs the ultrasound, will apply a water-based gel to the skin of the neck. This gel helps reduce air pockets between the ultrasound probe (also known as a transducer) and the skin, ensuring that the ultrasound waves can be transmitted effectively into the body.
Scanning Process: The sonographer moves the transducer back and forth across the neck. The transducer emits high-frequency sound waves that pass through the body and bounce back when they hit a boundary between tissues. These returning sound waves are then converted into images of the internal structures of the neck. The ultrasound machine has a screen that displays these real-time images.
Image Analysis: The sonographer looks at the ultrasound images on the screen to assess the size, shape, and structure of the lymph nodes and other neck structures. A color Doppler ultrasound may also be used to examine the blood flow in the neck, which can provide additional information, especially when assessing lymph nodes for signs of inflammation or cancer.
Completion: Once the sonographer has captured all the necessary images, they gel will be wiped off the patient’s neck. The whole procedure usually takes about 15-30 minutes.
Reporting: The images captured during the ultrasound are usually reviewed by a radiologist, a specialist doctor who interprets imaging studies. They analyze the images and write a detailed report outlining the findings.
One of the significant advantages of a neck ultrasound is its non-invasive and painless nature. It does not involve any needles, incisions, or injections, making it a simple procedure for both adults and children. From preparation to completion, the entire process causes no discomfort or pain. The transducer simply glides over the skin, and the patient typically feels only the mild, cool sensation of the ultrasound gel.
While ultrasound is an invaluable tool for assessing neck structures, it is operator-dependent, meaning the quality of the examination relies heavily on the skill and experience of the sonographer and the interpreting radiologist.
What Structures Does A Neck Ultrasound Evaluate?
A neck ultrasound can be used to evaluate various structures in the neck. The specific structures examined may depend on the patient’s symptoms, but generally, a neck ultrasound can evaluate the following:
Lymph Nodes: The neck has numerous lymph nodes, and ultrasound can assess their size, shape, and internal structure. Changes in these features may indicate infections, inflammatory conditions, or malignancies like lymphoma or metastatic cancer.
Thyroid Gland: Located in the lower part of the neck, this gland produces hormones that regulate metabolism. An ultrasound can detect abnormalities such as nodules, cysts, inflammation, or tumors in the thyroid.
Parathyroid Glands: These are four small glands located near or on the thyroid gland. They regulate calcium levels in the body. Ultrasound can help identify enlarged parathyroid glands, which can indicate a condition called hyperparathyroidism.
Blood Vessels: The carotid and vertebral arteries, which supply blood to the brain, can be evaluated with Doppler ultrasound to identify any blockages, narrowing, or other vascular conditions.
Soft Tissues: The ultrasound can evaluate the muscles, fatty tissues, and other soft structures in the neck for any abnormalities, such as cysts or tumors.
Larynx and Pharynx: While these structures are often better evaluated with other methods, a neck ultrasound can sometimes provide useful information about these parts of the throat.
What Ultrasound Features Can Be Seen? Short Axis? Fatty Hilum?
When examining a lymph node via ultrasound, two key measurements are taken into consideration – the long axis and the short axis of the lymph node. The short axis of a lymph node is essentially the diameter of the node measured at its widest point perpendicular to the long axis. While the long axis gives us the overall size of the lymph node, the short axis can provide a more accurate representation of the node’s shape and contour, which can be critical in assessing any abnormalities. 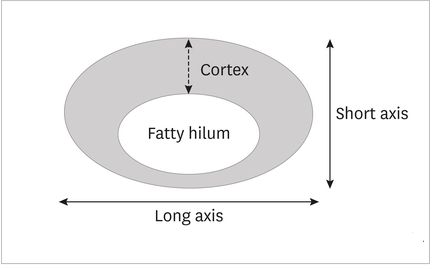
The internal structure of the lymph node affects its appearance on ultrasound, which includes the fatty hilum. The term ‘fatty hilum’ refers to a central area in the lymph node filled with fat cells, blood vessels, and efferent lymphatic vessels. The fatty hilum serves as a reference structure that reflects echoes on ultrasound images and is generally seen as a bright or white area in the center of the lymph node.
The presence of a fatty hilum is generally associated with normal lymph nodes, but its absence can sometimes signal potential pathology. Lymph nodes with a fatty hilum in the neck are usually considered to be reactive or benign. They have a smooth, oval shape with the hilum positioned centrally. However, their size can vary, but normal cervical lymph nodes usually do not exceed 10mm in the short axis on an ultrasound.
However, in certain conditions like lymphoma, the lymph node structure may appear altered on an ultrasound. A lymphoma lymph node might be larger in size, lack the typical fatty hilum of a normal lymph node, and can often appear hypoechoic, meaning it reflects fewer ultrasound waves and looks darker on the ultrasound image.
While the absence of a fatty hilum might raise suspicions of malignancy, it is not conclusive evidence of cancer. Cancerous lymph nodes on ultrasound often present with other features, such as round shape, loss of the fatty hilum, increased vascularization, and a larger size, especially in the short axis.
The importance of the fatty hilum and the short axis in lymph node ultrasound cannot be understated. They provide crucial clues to differentiate between benign and malignant lymph nodes and inform subsequent diagnostic and therapeutic steps.
Benign vs Malignant Lymph Node Ultrasound Of The Neck
What are specific ultrasound characteristics that define a benign node, versus a malignant node, specifically in the head and neck region?
Benign nodes on normal cervical lymph node ultrasound have a specific set of characteristics. They are usually oval or bean-shaped with the short axis less than half of the long axis. Although lymph node sizes can vary, the normal size of lymph nodes in the neck usually does not exceed 10mm in short axis diameter. The periphery of the node is usually smooth and well-defined.
A fatty hilum is one of the features that distinguishes a benign lymph node from a malignant one on ultrasound. The fatty hilum, also known as fatty hila in the plural form, appears as a bright or white area in the center of the lymph node. This acts as an echoic reference structure; and is also a crucial landmark when performing an ultrasound. A lymph node with fatty hilum, or lymph nodes with fatty hila are more likely to be benign in nature.
In addition, a feature referred to as ‘cortical thinning’ may also be evident in normal lymph nodes. This means that the outer layer, or the cortex, of the node is thin, typically measuring less than 3mm. Normal nodes will not have any nodular or irregular extensions in the cortical layer. The cortical layer is generally also distributed evenly around the fatty hilum of the lymph node.
Contrastingly, an abnormal lymph node ultrasound may have several features which can be suggestive of an abnormal or potentially cancerous node. Many mentions have been made of the short axis of the lymph node and its implications. A round lymph node, where the short axis measures greater than half the size of the long axis, may potentially be suspicious. Any significant increase in the size of the lymph node, measured as when the short axis exceeds 10mm, could also be deemed suspicious.
An abnormal or malignant lymph node may also lack the typical bright or white appearance of the fatty hilum; or may appear as a lymph node without a fatty hilum. Instead, the node may be more hypoechoic, meaning it reflects fewer ultrasound waves and appears darker on the ultrasound image.
Another crucial feature which may indicate malignancy is cortical thickening. This occurs when the cortex of the node appears to be thicker than 3mm and is unevenly distributed around the hilum. In some cases, it may display a nodular or irregular pattern.
Increased blood vessels or blood flow within the node can also be a sign of pathology. Lymph nodes battling infections or malignancies may show more blood flow, visible as color signals when using Doppler ultrasound.
However, these features are in no way definitive. An ultrasound assists the physician in making a decision as to whether additional investigations, such as fine needle aspiration cytology (FNAC) for cancer cells or biopsy are required to confirm the diagnosis. At the end of the day, the combination of clinical evaluation, ultrasound findings and if necessary, further investigations guide diagnosis and patient care.
| Feature | Benign Lymph Node | Malignant Lymph Node |
|---|---|---|
| Shape | Oval or bean-shaped | More round in shape |
| Size | Short axis usually less than 10mm | Short axis often greater than 10mm |
| Fatty Hilum | Visible and centrally located | Often absent or displaced |
| Cortex | Thin, usually less than 3mm | Thickened, often more than 3mm |
| Echogenicity | Homogeneous echotexture | Heterogeneous or hypoechoic |
| Vascularity (Doppler) | Central vascularity | Increased and peripheral vascularity |
| Margin | Smooth and well-defined | Irregular and poorly defined |